Immuno-oncology provides hope to cancer patients
Seen as a major breakthrough in cancer treatment, immuno-oncology could be the hope the world has waited for
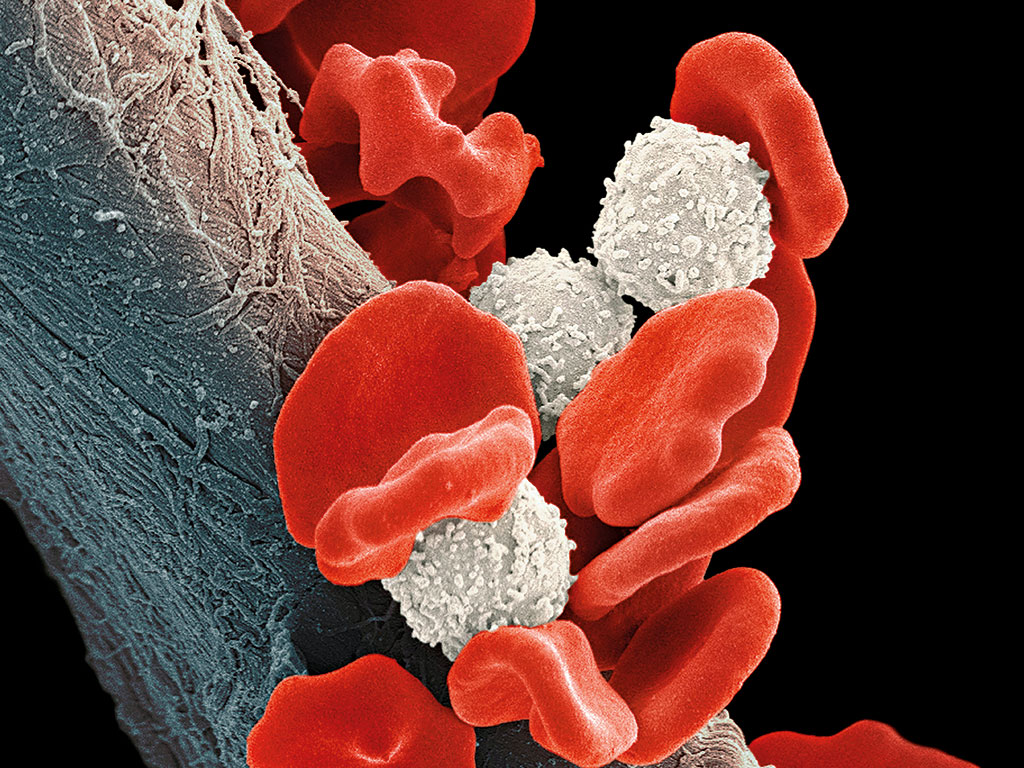
Immuno-therapy uses the body's natural defence mechanisms to fight cancer, without causing harm to healthy cells
Cancer survival rates have improved considerably in recent decades thanks to ongoing research and recent advances; in the UK for example, they have doubled in the past 40 years, according to NGO Cancer Research UK. That being said, the disease still affects millions of people around the world each year, regardless of age, ethnicity and economic standing. There are various well-known methods for treating patients, including chemotherapy, radiotherapy and surgery, as well as other hopeful new types of medication. While such treatments are effective in their own ways, each presents its own challenges via harmful side effects that can be as dangerous as the disease itself.
But now there is an alternative method: one that combats cancer in a completely different way from its predecessors and potentially heralds a revolutionary era in treatment. First conceived in the 1970s, immuno-oncology uses the body’s natural defence mechanisms to fight cancer, without causing harm to healthy cells. So far, immunotherapy drugs have brought about remission in inoperable cancers and an impressive extension of life expectancy for terminally ill patients. Given their effectiveness, the entire pharmaceutical sector has taken note, from private investors to multinational firms that can afford the pricey studies.
Natural defence mechanism
Over the last decade, there has been a significant improvement in the cancer medication that is available on the market. Newer drugs are far better at targeting tumours, providing greater efficacy while also reducing the assault on healthy cells, thereby causing fewer damaging side effects for patients. Although ‘targeted drugs’ showed promise as a miracle breakthrough when first unveiled, they have since disappointed due to the persistent adaptation of cancerous cells and their ability to build drug resistance.
21%
Of patients were alive three years after treatment with ipilimumab
$150,000
Cost of a checkpoint inhibitor per patient per year
$20-30bn
Potential annual cost of checkpoint inhibitors by 2025
To combat this impediment to remission, research continued on harnessing the immune system to fight cancer. Although vaccines again showed disappointing results, they prompted a pivotal breakthrough. “This [research] led to the discovery that cancer cells use a ‘checkpoint’ signal to fool the immune system into thinking that they are healthy cells, so the immune system won’t kill them”, said Stephen Dunn, Senior Managing Director of Research for LifeTech Capital. In the early 1990s, scientists in Japan discovered the molecule on T-cells (a type of white blood cell) that enables cancer cells to ‘hide’ from attack. Naming the molecule ‘programmed death 1’ (PD-1), they began research on how to disrupt the mechanism. “The newest immuno-oncology drugs that have been making headlines are designed to block this immune checkpoint signal – [they] are called ‘checkpoint inhibitors’”, Dunn added. “The impact of this new mechanism is not just evolutionary, it’s revolutionary”.
By blocking checkpoint inhibitors, immunotherapy drugs can eliminate the very problem that has limited success in cancer research thus far. “It turns out that our immune system is quite effective in killing cancer cells once the brake is released”, said Dunn. “The result is not only an entirely new mechanism of action against cancer cells, it opens the door for even more efficacy when used in combination with existing drugs to perhaps make them work even better.”
New immunotherapy drugs are also far better than traditional counterparts at providing a long-term memory. This means that, as cancer cells adapt over time, the immune system will continue to attack, providing a long-lasting, durable response, even after remission.
Research carried out so far also shows immuno-oncology drugs are effective against the more difficult-to-treat and inoperable cancers, such as melanoma, a type of skin cancer that can spread to other organs in the body.
“The immune system is programmed to recognise danger from the outside world”, said Peter Johnson, Professor of Medical Oncology at the Cancer Research UK Centre in Southampton General Hospital. “The most heavily mutated cancers appear different from normal cells because they give off more danger signals than cancers with fewer mutations. Paradoxically, this makes the most difficult cancers to treat with things such as chemotherapy and radiotherapy much more susceptible to immune treatments.”
Captivating investment
First to receive FDA approval for immunotherapy drugs in treating metastatic melanoma was Bristol Myers Squibb with Yervoy (ipilimumab) and Opdivo (nivolumab). One study has shown 21 percent of 4,846 patients analysed were still alive three years after treatment with ipilimumab, despite previous predictions they would not survive otherwise. Opdivo, a PD-1 blocker, has had exciting results in terms of shrinking tumours; in March, it was also approved for the treatment of advanced squamous non-small cell lung cancer (NSCLC), a significant step given lung cancer is the leading cause of cancer death worldwide, according to the Cancer Research Institute. The next step that is expected to further boost sales of Opdivo is FDA approval for the less common type of lung cancer, non-squamous NSCLC.
Small biotechnology firms are making headway in immuno-oncology research
Although the two drugs have shown promising outcomes separately, when they are used together as part of a combined therapy course the results have been exceptional. According to a press release published by Bristol Myers Squibb, in one trial the combined regimen achieved a 61 objective response rate. “The two drugs work better in combination because they disinhibit the immune system at different places in the process, so the effect is to release the immune response much more completely”, Professor Johnson explained. Another Bristol Myers Squibb study showed a median of 945 patients lived for 11.5 months without the disease progressing, in comparison with 6.9 months for Opdivo alone and 2.9 months for Yervoy.
Bristol Myers Squibb may be leading the way in immuno-oncology at present, but it is not alone in its recent ventures. Pharmaceutical giant Merck also has its own version of the Opdivo drug called Keytruda, which has received FDA approval for melanoma, with NSCLC treatment currently under review.
Considering the mammoth cost of investment and research required to carry out the studies and tests needed for the sector, it is mostly restricted to the biggest players in the pharmaceutical industry. That being said, various small biotechnology firms are making headway in immuno-oncology research. Maryland-based Northwest Biotherapeutics, for example, is running trials with its DCVax vaccine, a platform technology that uses dendritic cells to educate the entire immune system to attack cancerous ones.
The cost of the treatment has sent waves through the investment market for both positive and negative reasons. Dunn said: “At the present time, the pricing for a checkpoint inhibitor is approximately $150,000 per year per patient in the US, so the financial impact for the companies (as well as healthcare costs) is expected to be significant, perhaps $20bn to $30bn annually by 2025. Those numbers are large enough to ‘move the needle’ for even the largest pharmaceutical companies and have investors excited.”
As a result of the recent surge in immuno-oncology investment, the sector now has its own stock index: the Loncar Cancer Immunotherapy Index (LCINDX), named after founder and owner Brad Loncar. The equal-weighted index currently contains 30 companies, ranging from large pharmaceutical corporations to smaller growth biotechnology firms. All firms included in the index have a high focus on immuno-oncology and, as LCINDX provides a metric for their progress, it gives investors a more focused understanding of a sector that is expected to expand considerably over the next decade.
As quantified by Dunn, the potential is huge. However, the extraordinary prices could also be the downfall for this promising new sector. Such expensive treatment will undoubtedly be out of reach for many patients, particularly in countries such as the US, while in countries where there is a national health service, immuno-oncology treatment may be denied due to restrictions on the state budget.
Just the start
Melanoma and lung cancer are just the beginning. “We anticipate that these treatments may be effective in cancers such as oesophageal, bladder, head and neck, renal, and some types of bowel cancer in particular”, said Professor Johnson. “They are also very active against Hodgkin lymphoma, although they may be working in a different way there, by disrupting the signalling between the malignant cells and their surroundings.”
Ludwig Cancer Research, a leader in the field having helped lay the foundations of immuno-oncology, is currently undertaking a number of innovative studies across the globe. “Various Ludwig researchers at Harvard, Stanford, Oxford, and in Brussels, New York and Chicago (and other places) are involved in the full spectrum of research related to immuno-oncology, from identifying new molecular and immune cell targets to assessing new therapeutic strategies that include immunotherapies”, said Jonathan Skipper, Executive Director of Technology Development at Ludwig. “A new Branch [of] Ludwig [that] just launched in Lausanne is going to be almost exclusively involved in developing novel immunotherapies, with a special emphasis on developing individualised, cell-based therapies and the processes required to put such therapies to routine use”.
It doesn’t end there: iTeos, a Ludwig spin-off is focusing on the development of small molecule drugs that block a key metabolic mechanism that usually silences the immune response in tumours. “In partnership with the Cancer Research Institute, Ludwig is also evaluating an immunotherapy for the treatment of glioblastoma multiforme, the most aggressive adult brain cancer”, said Dr Jedd Wolchok, a member of Ludwig at MSK. “Another trial in this partnership will be looking at combining PD-1 blockade and CTLA-4 blockade for a variety of solid tumours, including those of ovarian cancer, colorectal cancer, cervical cancer and kidney cancer. But all this is only the beginning of what I believe will be a very exciting era for oncology.”
Medical revolution
Immuno-oncology is still evolving, with many questions yet to be answered, such as understanding why the treatment works in some patients, but is not effective in others.
The single biggest cause of cancers – smoking – also results in the most dramatically mutated genomes
“As might be expected, people whose cancers express PD-1’s binding partner, PD-L1, respond more frequently to PD-1 blockade than those whose tumours do not”, said Dr Wolchok. “We and other researchers have also found rather consistently that, in the case of checkpoint blockade at least, patients with more mutated cancer genomes are more likely to respond to the treatments. This is very exciting, since the single biggest cause of cancers – smoking – also results in the most dramatically mutated genomes.
“We are also focusing on what particular mutational signatures in tumours elicit robust therapeutic responses with these therapies. Another Ludwig researcher at Johns Hopkins recently showed that tumours in which the genes for DNA repair are mutated respond dramatically to checkpoint blockade. But this work is just beginning, and we can expect a lot of very interesting information to come out of such research in the next few years.”
There is also a great deal of research to be carried out into using immunotherapy for other types of cancer, not to mention the various regulatory hurdles before they can reach the market. “We are just at the beginning of this field. We have much to learn about what affects susceptibility to immunotherapy, and how we can increase the effectiveness by combining antibodies, vaccines, small molecule immune-modulators and other types of treatment”, Professor Johnson explained.
Greater understanding is needed urgently to explain why serious side effects – which can be so bad they require the cessation of treatment – can occur. For Opdivo, they include fatigue, loss of appetite, nausea, musculoskeletal pain and constipation, according to the FDA. But they can also be far more serious: in one patient who suffered from advanced melanoma, treatment with Yervoy resulted in “off the chart” presence of an enzyme that can cause grave damage to muscles, leading to his hospitalisation for possible kidney failure. Moreover, although combining Yervoy and Opdivo improves the response of the immune system, together they can also cause more potent side effects.
“A clearer understanding of who benefits from immunotherapy combinations may allow for a better risk-benefit profile, especially as combination therapies have more frequent, yet generally reversible toxicities”, said Dr Wolchok. “In the area of individualised, cell-based immunotherapy, which has great potential, we have to figure out how such treatments can be standardised, streamlined and made affordable for general clinical deployment. That will not be easy.”
While there are still challenges and hurdles to overcome, as with any advancement in medicine and particularly one as complex as this, immuno-oncology is still hailed by many as the long-awaited breakthrough in cancer treatment.
“I expect the immuno-oncology field to ultimately revolutionise treatment for cancer patients, both in terms of survival and quality of life”, said Dunn. “While it is making headlines now, I believe the greatest discoveries still lie ahead in combination with other drugs that work in conjunction with the patient’s immune system.”
And Dunn is not alone in this thinking. Dr Wolchok said: “I think we have, for the first time, good reason to be optimistic that we’ve found in immunotherapy a way to durably control many types of cancer that have historically been invariably and swiftly lethal.”
By identifying how cancer cells adapt and hide from the body’s defence mechanisms, scientists are finally able to unlock the missing link that has eluded researchers for decades. This key opens up a whole new world of possibilities for cancer treatment. With investors lining up to participate in the sector and given the enthusiasm shown by research centres and pharmaceutical companies both large and small, the rate of new discoveries in immuno-oncology could be exponential. As Dunn said: “While perhaps not yet a cancer cure, we may be able to turn cancer from being a terminal disease into just a chronic disease, like diabetes or arthritis. The best is yet to come.”













