While manageable, the process of daily insulin injections for type 1 diabetics is an inconvenience to say the least. The need to monitor insulin levels with frequent, inconvenient tests is the only option available to a number of people, impacting on freedoms and quality of life. This could soon change though, thanks to an innovative solution currently in development.
Research being undertaken with the assistance of Ingenuity Lab in the field of pancreatic islets transplantation could lead to type 1 diabetics having to worry less about their condition. Between the use of an alternative cell source to humans and the development of a scaffold that will support the growth of transplanted cells, implanting islets could finally become a practical solution.
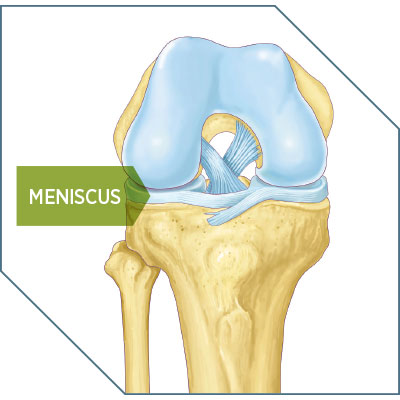
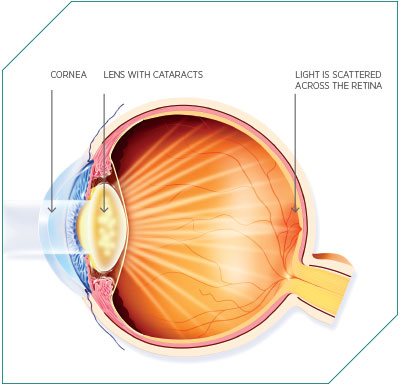
Type 1 diabetes occurs when the pancreas, a small gland located behind the stomach, fails to produce the correct level of insulin a person needs. Insulin is a hormone that maintains blood-glucose levels in the body, and subsequently energy levels. If the body is failing to manage its energy levels correctly, it leads to a range of short-term problems, such as tiredness and weight loss. Long term, the effects are far more damaging, with potential issues ranging from kidney disease, heart disease, blindness and possible limb amputation. Apart from injections of insulin to keep levels correct, alternative treatments are often underdeveloped: an insulin pump via which the hormone can be administered, for example, is only practical for a relatively small number of patients. Another therapy alternative has been the transplantation of pancreatic islets. This solution might seem like an obvious one, but logistically it has always been impractical; as with any transplant therapy, there is a constant shortage of donors. Public awareness and education programmes can only go so far. However, a new source of cells is being investigated.
Continuing legacy
Dr Gregory Korbutt at the University of Alberta is carrying out research on an alternative source of islets, as well as a new way to implant them.
“One of the things we’ve developed here is using pigs as the source of insulin-producing cells”, said Korbutt. Pigs are a common candidate for human transplantation thanks to their availability, comparably sized organs and their genetic distance from humans. The work carries on the legacy of groundbreaking pancreatic research conducted at the University of Alberta. The school was the first to develop a standard for the implantation of islets, known internationally as the Edmonton Protocol, in a paper published in 2000. Korbutt, who was part of that original research team, said that, while the initial protocol recommended islets be transplanted into the liver, new research is now indicating there could be a better location. Along with the cell source, Dr Korbutt is also currently working on finding a better way to implant the cells.
“Then we are combining it with the technology from Ingenuity Lab”, he explained. “They’re able to make biomaterials. Ultimately, it would be a very non-invasive procedure if we were able to develop a transplant site – let’s say underneath the skin of patients. And that’s where Ingenuity Lab with their biomaterials are very useful.”
The islet transplantation doesn’t represent a cure for type 1 diabetes, but it could make living with the condition a far more manageable experience.
“It’s changing one form of therapy for another”, said Korbutt. “Instead of taking daily insulin injections, you’re getting a transplant. Seeing as it is a transplant, patients have to take anti-rejection drugs. But that’s where these biomaterials come into play.”
The research theorises that the use of a scaffold could create a space within the body that would receive enough blood flow to encourage transplanted pancreatic islets to graft onto their new host, survive and then begin producing insulin.
This is a challenge in two halves. The first is the source of pancreatic islets, which Korbutt is working on, but the second is the scaffold. This is the key to encouraging the cell growth that is needed for the transplanted cells to survive for any worthwhile amount of time. This is the portion of the project Dr Sinoj Abraham from Ingenuity Lab is working on.
New materials
Abraham said, when it comes down to it, the material of the scaffold makes all the difference. “The biomaterials we are making basically mimic the growth factors in the body, and then we also make the polymers with the different combinations. We customise the polymers so that we could easily customise it depending upon the patient, depending on the degradability, and all those things.”
What has made this innovation possible is the development of new materials that have a biological function built into them. Scaffolds used to be basically just a frame, with the patient's body having to develop its own growth factors. New materials can mimic the growth factors of the human body, so the process for the transplant integrating with the patient’s body becomes faster.

“We’re going to develop strategies where we can modify these biomaterials by putting molecules on that will help prevent rejection, and then the patients wouldn’t have to take lifelong anti-rejection drugs”, said Korbutt.
Pancreatic research is a competitive field to be working in, with several different strategies to solving the same problem currently in the works. One such project is the artificial pancreas, an electronic device that remotely checks glucose levels through a sensor placed under the skin. It wirelessly transmits information to a monitor worn on the body, and then transmits that information to a pump that maintains insulin levels.
Korbutt said, while the research is exciting, the technology isn’t quite there yet. “The problem with the artificial pancreas is the technology is not there to have a sensor that can detect patients' blood sugar and to release the insulin.”
The research partnership between Korbutt and Ingenuity Lab is still in its early days, but the collaboration has already found some traction with outside parties. “We established this collaboration I would say approximately nine months, so I would say that we are just starting”, said Korbutt. “We have just recently got funding from the Juvenile Diabetes Research Foundation, which is an international organisation that funds research into type 1 diabetes.”
Despite the challenges the research presents, Korbutt said he is confident the challenges can be overcome. “It’s research, so there’s always going to be barriers, but in research you do the experiment, if they don’t work you modify them and then you proceed. I think that a novel thing that we have here is we’re combining the biology with the biomaterial engineering expertise.
“In research, one group cannot solve all the problems, and that’s, I think, the novel part of this: we’re combining technologies. It strengthens the project and I feel will improve the probability of succeeding.”